Breast cancer is a complex and aggressive disease that affects millions of women worldwide. While chemotherapy has long been considered a standard treatment option, many patients develop resistance to these medications, leading to suboptimal outcomes. Recent research has shed light on the importance of the tumor microenvironment in mediating chemotherapy resistance in breast cancer. In this blog post, we will explore the mechanisms behind this resistance and discuss how insights from the tumor microenvironment can pave the way for novel therapeutic strategies.
The Role of Tumor-Associated Immune Cells
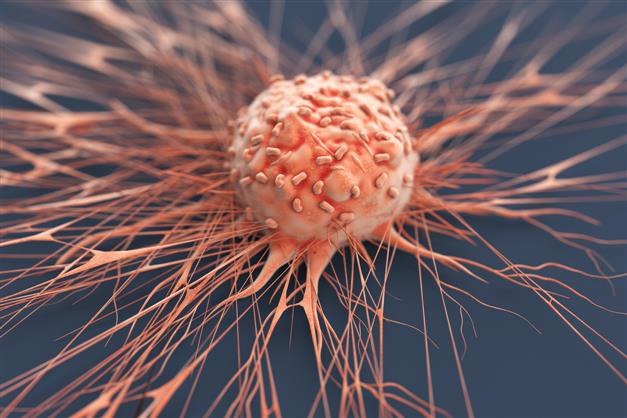
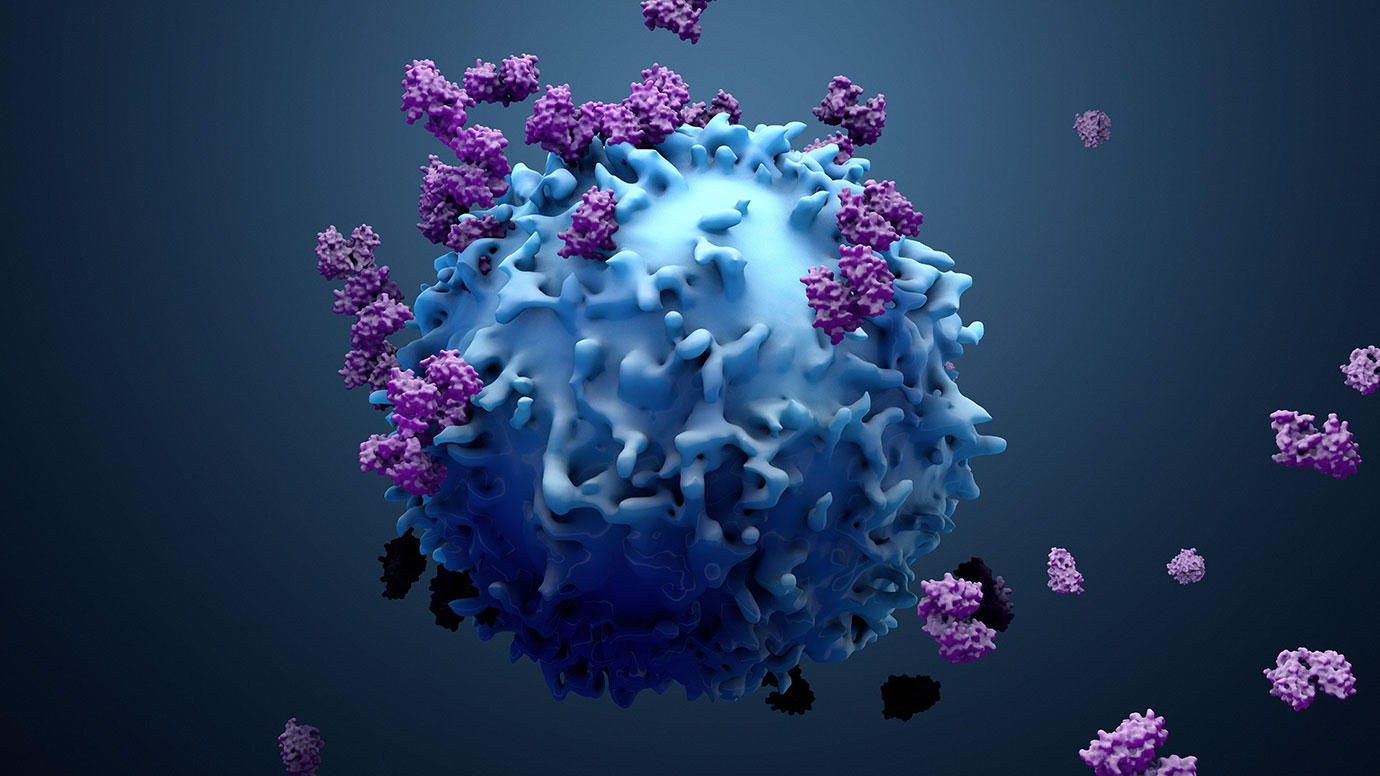
Tumor-associated immune cells play a crucial role in modulating the response to chemotherapy in breast cancer. One mechanism by which they contribute to resistance is through their ability to create an immunosuppressive microenvironment within the tumor. This can be achieved through several means, such as the recruitment and activation of regulatory T cells, myeloid-derived suppressor cells (MDSCs), and M2 macrophages. These immune cell subsets release factors that suppress anti-tumor immune responses and promote tumor growth.
Another way in which tumor-associated immune cells contribute to chemotherapy resistance is by directly interacting with cancer cells. Studies have shown that some immune cell populations express drug efflux pumps such as P-glycoprotein, which functions to pump out chemotherapeutic agents from cancer cells before they can exert their cytotoxic effects. Additionally, these immune cells can secrete growth factors and cytokines that promote survival pathways in cancer cells.
Emerging evidence also suggests that tumor-associated immune cells may have diverse phenotypic states within different regions of a single tumor or among distinct tumors within an individual patient's body. This phenotypic heterogeneity creates challenges for targeted therapy development but also opens up opportunities for combination approaches targeting multiple immunological mechanisms.
Impact of Cancer-Associated Fibroblasts
Cancer-associated fibroblasts (CAFs) are another component of the breast tumor microenvironment that can contribute to chemotherapy resistance. CAFs are activated fibroblasts that undergo phenotypic changes in response to signals from cancer cells and the surrounding stroma. These cells have been shown to promote tumor growth, invasion, and metastasis through the production of extracellular matrix components and growth factors.
Studies have indicated that CAFs can protect cancer cells from the cytotoxic effects of chemotherapy drugs by creating a physical barrier around them. This barrier hinders drug penetration into the tumor, rendering the cancer cells less susceptible to treatment. Furthermore, CAFs can secrete chemokines that recruit immune-suppressive cells into the tumor microenvironment, further exacerbating therapy resistance.
Targeting CAFs is therefore being explored as a potential strategy to overcome chemotherapy resistance in breast cancer. Several preclinical studies have demonstrated promising results by using inhibitors or genetically modifying these cells to inhibit their pro-tumorigenic properties. However, more research is needed to fully understand how CAFs interact with other components within the tumor microenvironment and how they might be precisely targeted for efficient therapy.
Microenvironmental Factors Influencing Chemotherapy Response
Apart from immune cells and fibroblasts, various other microenvironmental factors contribute significantly to chemotherapy resistance in breast cancer. The hypoxic nature of solid tumors has been associated with poor responses to chemotherapeutic agents as low oxygen levels promote drug resistance pathways within cancer cells.
Additionally, alterations in cellular metabolism observed within tumors also influence chemotherapy response. Cancer cells often exhibit enhanced glucose uptake and reliance on anaerobic glycolysis even under normoxic conditions (known as the Warburg effect). This metabolic reprogramming not only provides energy for rapid proliferation but also renders breast cancer cells resistant to certain types of chemotherapy drugs like taxanes.
Furthermore, genetic alterations occurring within specific cell populations in the tumor microenvironment can also impact treatment response variability between patients. For example, mutations affecting DNA repair mechanisms can lead to increased resistance to DNA-damaging agents like anthracyclines.
In conclusion, breast cancer chemotherapy resistance is a multifactorial phenomenon that involves various components of the tumor microenvironment. Tumor-associated immune cells, cancer-associated fibroblasts, and microenvironmental factors all contribute to the development of resistance and play crucial roles in determining treatment outcomes. Understanding the mechanisms behind chemotherapy resistance in breast cancer will aid in the development of novel therapeutic strategies that target these microenvironmental interactions, ultimately improving outcomes for patients with this devastating disease.